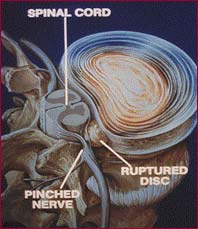
Cauda Equina Syndrome: This is a massive herniation causing altered bowel or bladder control and sometimes paralysis. Although rare, this entity is a surgical emergency.
Progressive Neurological Deficit: This refers to a disc syndrome in which neurological abnormalities such as weakness, numbness, reflexes, etc., are documented to deteriorate over time. A neurologic deficit which is present but not deteriorating can be observed without surgery. Neurologic deficits associated with disc herniations are common but progressive deficits are uncommon.
Persistent Severe Pain: This is another indication for surgery but often medication, epidural shots and other pain-control treatments can be used to control symptoms so that conservative care can be tried.
The decision to do surgery is based primarily on the physical exam, not the MRI or CT scan. In fact, some of the worst looking disc herniations on scans produce very little and sometimes no symptoms at all (more details on asymptomatic disc herniations). Furthermore, large disc herniations often shrink and totally disappear on scans reflecting the body’s ability to heal.
Some reasons to avoid surgery include:
- Even if all appropriate criteria are met, the operation sometimes does not relieve the pain.
- Surgery can lead to scar tissue causing permanent symptoms not amenable to treatment.
- The risk of infection, anesthesia and hospitalization.
- In some cases surgery can lead to a “post-discectomy syndrome” where, despite some initial improvement, symptoms recur eventually requiring more surgery. The surgeons are constantly trying to improve their techniques to minimize these issues but they still ex.
- Studies reveal that patients symptoms are about the same a few years after a “disc syndrome” whether or not they have undergone surgery.
Few patients want surgery but they also are concerned that if they refuse they might suffer permanent damage. Two large government funded studies have addressed this question providing more information to help patients make informed decisions.
Specialized Spine Care has developed a conservative treatment program for patients with disc syndromes who do not need immediate surgery. It involves a very controlled, supervised light exercise program designed to specifically improve the healing physiology in the affected disc area and prevent recurrences through specific strengthening.
As symptoms improve, exercise intensity is increased in order to normalize any strength deficits in the back or neck. This is very important because after spine injuries patients are at risk for recurrence. Medical evidence suggests that spinal deconditioning may be an important factor in this increased risk. Finally, we recommend that post-surgical patients get their back strength tested and, if weak, consider the program for these very same reasons. Check out our neck pain relief service